
Reporting of sentinel events to The Joint Commission is a voluntary process, and no conclusions should be drawn about the actual relative frequency of events or trends in events over time.

The remaining sentinel events were reported either by patients or their families, or employees of a healthcare organization. The majority of sentinel events (90%) were voluntarily self-reported to The Joint Commission by an accredited or certified healthcare organization. Such an event is an unexpected occurrence involving death or serious physical or psychological injury, or the risk thereof. Our goal is to help prevent these types of adverse events from occurring again.” The Joint Commission on the Accreditation of Healthcare Organizations (JCAHO) requires the reporting of sentinel events. “For each sentinel event, a Joint Commission patient safety specialist worked with the impacted healthcare organization to identify underlying causes and improvement strategies. “COVID-19 continued to present challenges to healthcare organizations throughout 2022, and we saw the number of sentinel events increase above pre-pandemic levels,” notes Haytham Kaafarani, MD, MPH, FACS, chief patient safety officer and medical director, The Joint Commission. Of all the sentinel events, 20% were associated with patient death, 44% with severe temporary harm and 13% with unexpected additional care/extended stay. Patient falls were the most common sentinel event reported among hospitals in the first six months of 2022, according to a Sept. Most reported sentinel events occurred in a hospital (88%).

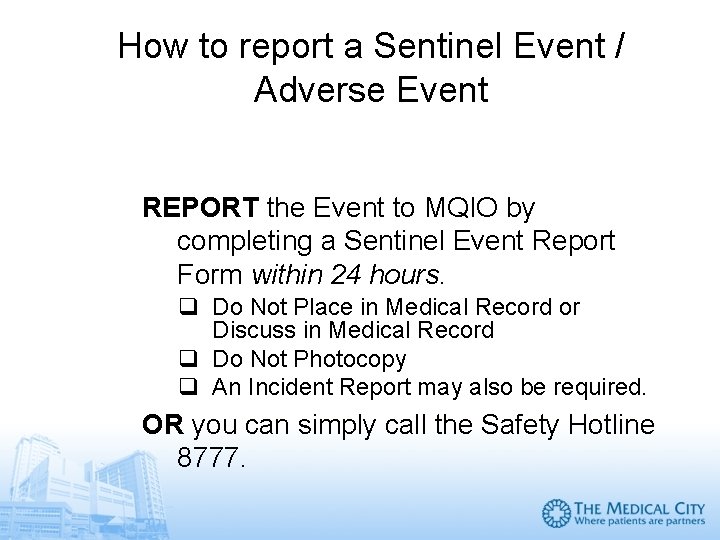
A sentinel event is a patient safety event that results in death, permanent harm or severe temporary harm. Traditional efforts to detect AEs have focused on voluntary reporting and tracking of errors.
The Joint Commission has released its Sentinel Event Data 2022 Annual Review on serious adverse events from Jan.


 0 kommentar(er)
0 kommentar(er)
